Home » Health Education » Peripheral Artery Disease
What is peripheral artery disease?
Peripheral artery disease, or PAD, is a condition where the restricted arteries reduce the flow of oxygenated blood to the limbs. Symptoms range from mild to acute and it is treatable as well as preventable with the right lifestyle habits. In this article, you can learn everything you need to know about PAD and how it may affect your quality of life.
How your circulatory system is supposed to work
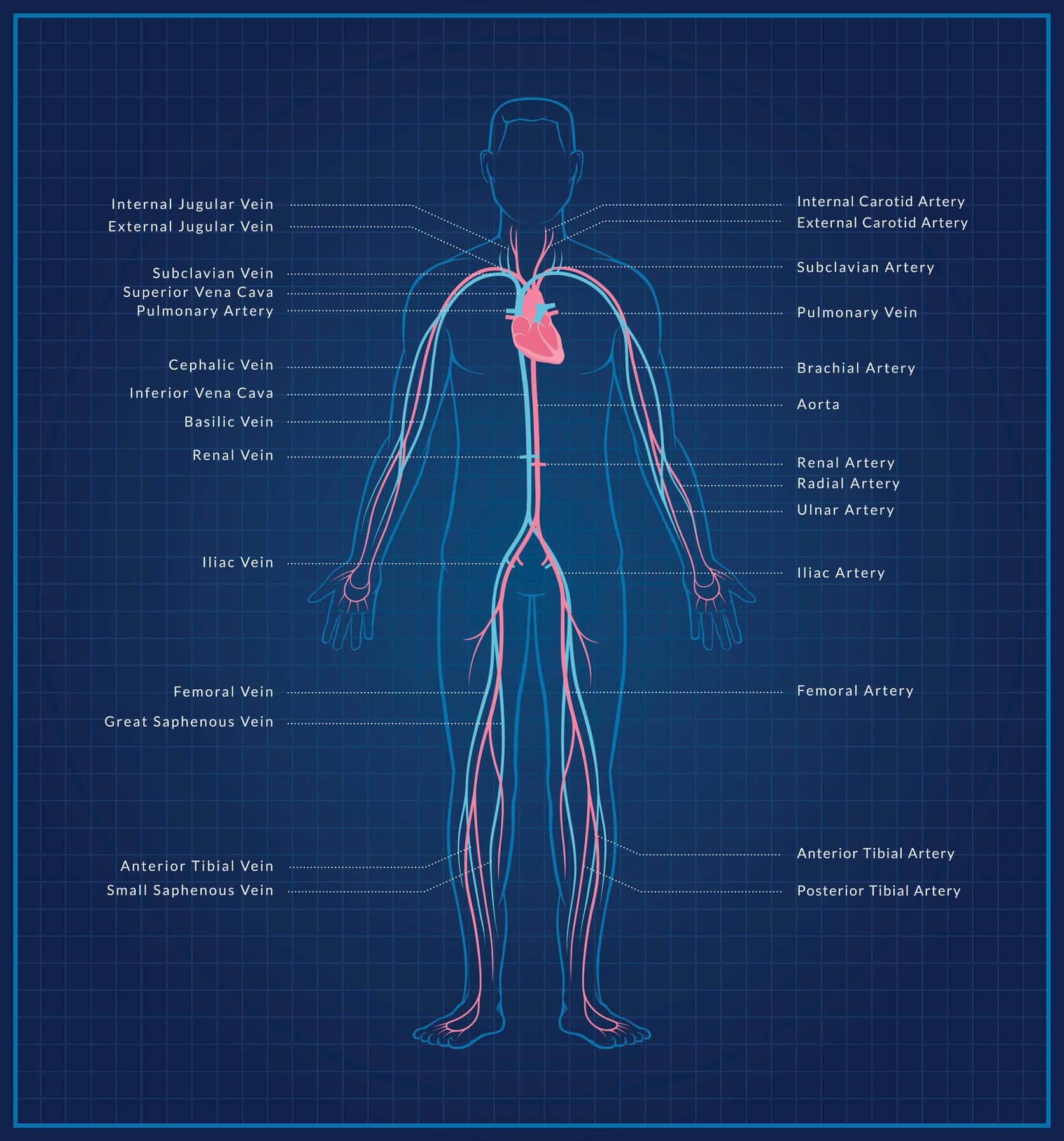
In order to talk more about PAD and why it affects people the way it does, it helps to have a basic understanding of the circulatory system and how it works. When you breathe in, oxygen goes into your lungs. Your heart then pulls in that oxygen and infuses it into the blood that is running through it. Oxygen-poor blood is carried to your heart by blood vessels called veins while the oxygen-rich blood is sent out to the rest of your body through arteries.
Your peripheral arteries are the ones that extend to the parts of your body furthest from your heart: the arms and legs. Because blood has to travel the farthest to get here, the limbs are sometimes the first places an issue can arise.
What causes PAD?
Peripheral artery disease is caused by the buildup of arterial plaque in your blood vessels. This plaque is mostly made up of cholesterol and narrows the arteries, making it difficult for blood to pass through and get to your limbs where it is needed. With less room to travel, blood pressure increases and there is an increased risk of clotting. While PAD can occur in your arms, the vast majority of cases are found in the legs. This is most likely due to gravity and these being the lowest blood vessels in the body.
PAD is an extremely common cardiovascular disease, with 8.5 million cases in adults over 40 just in the U.S.. Depending on how advanced the case is, people have reported a variety of symptoms. In fact, it’s estimated that 20-50% of those with PAD show no symptoms at all.
Peripheral Artery Disease Symptoms
- Skin that is cool to the touch
- Constant leg pain, tingling, burning, or loss of all sensation
- Cramping in the calves, thighs and hips, especially after periods of activity
- Hair loss in the legs and feet
- Change in color in the legs
- Sores on the feet that won’t heal
- Slow toenail growth
- Erectile dysfunction
All of these symptoms can be traced back to a lack of adequate blood flow. For example, areas that aren’t getting enough blood circulation feel cool to the touch. Hair follicles require a steady supply of oxygenated blood to live and so, when they die, hair falls out. Your body needs fresh blood to heal and repair itself, which is why sores and cuts on the feet and legs won’t heal. This is complicated by the fact that you may be experiencing numbness, so you might not even be aware of any injury.
If you are experiencing any of these symptoms the best thing to do is get in touch with your physician. If the problem is PAD, they’ll be able to figure out the next steps toward getting you healthy again.
Who is most at risk for Peripheral Artery Disease?
Age is one of the most significant factors when assessing risk for PAD. It’s estimated that 15% of adults over the age of 70 have PAD. You can absolutely develop it when you are younger, but the older you are, the more you have to be aware of your risk. Beyond age, there are several other factors that can increase your risk to develop PAD.
Peripheral Artery Disease Risk Factors
High Blood Pressure
Those with high blood pressure are more likely to develop PAD, along with other cardiovascular diseases like carotid artery disease and coronary artery disease. Blood pressure can be managed through doctor-prescribed medication, exercising regularly and avoiding stress when possible.
Diabetes
1 in 3 diabetics over the age of 50 develop PAD. Also, the longer you’ve had diabetes, the more likely you are to develop PAD. Talk to your doctor about what extra steps you should be taking to lower your risk of developing cardiovascular disease.
Genetics
Family history plays a large part in your chance to develop peripheral artery disease. This is true for many health conditions, which makes it all the more important to investigate your family tree for any recurring diseases that you should be especially aware of.
Smoking
The chemicals in cigarettes are known to irritate arteries and cause them to become inflamed. When blood vessels swell they become more rigid and the passage for blood gets narrower. This increases blood pressure (another PAD risk factor) and increases the risk of clotting.
Kidney Disease
Studies confirm that there is a link between kidney health and cardiovascular disease. While this is true for all forms of atherosclerosis, recent studies have shown that those suffering from CKD are particularly at risk to develop peripheral artery disease.
Race
For reasons that aren’t completely understood, PAD is more common in African Americans than it is in other ethnic groups. While it is no guarantee, it does need to be factored in when considering how at-risk you are.
Obesity
Too much body fat can have a dramatic affect on the health of blood vessels, and your body in general. Excess body fat pushes on the arteries from the outside, squeezing them. This, in turn, creates the same narrow passageways and problems that come from smoking. Obesity also causes the heart to have to work harder to get blood throughout the body, causing additional strain on the whole system.
High Cholesterol Levels
Arterial plaque is primarily made up of cholesterol. When assessing your cholesterol levels, keep in mind there are two kinds: high-density lipoproteins (HDLs) and low-density lipoproteins (LDLs). HDLs are considered “good cholesterol”. These particles actively pull extra cholesterol from the artery walls. LDLs, on the other hand, deposit cholesterol in the artery walls.
How to know if you have peripheral artery disease
As we mentioned, many people have PAD and don’t know. Others may experience only mild symptoms and not take the condition seriously. However, the longer PAD is left untreated the worse it can get. The loss of blood flow to the legs can cause tissue death and, in extreme cases, require amputation.
Because a lot of people with PAD don’t experience any symptoms, screening for PAD is extremely important. You can’t fix a problem you don’t know about. Additionally, disease in the arteries of the legs often indicates issues in other areas of the body, like the arteries of the heart. Those with PAD are more at risk for other cardiovascular issues like coronary heart disease and carotid artery disease.
What is a peripheral artery disease screening?
Fortunately, there is a quick, easy test that can be performed to assess your arterial health. A PAD screening is a quick, non-invasive process. All you have to do is take off your shoes and socks, and the technologist will put blood pressure cuffs on your ankles and upper arms. It’s a process similar to having your blood pressure taken at the doctor’s office or self-service machine at the store.
The measurements taken from your arms and legs are used to calculate the ankle-brachial index (ABI), which compares the blood pressure at your ankle to the blood pressure at your arm. If that number falls outside the normal range of 1–1.3, you might be at risk of developing PAD. But even if your screening ABI falls within the normal range, if you are having symptoms such as pain in your legs that feels better after resting, you should see your doctor.
If your screening ABI is outside the normal range, you should reach out to your doctor and let them know. You’ll need to schedule a visit so he or she can determine if any additional testing or treatment may be necessary.
What if I have peripheral artery disease? Can I do anything about it?
The goal of treatment for PAD is to reduce the risk of heart attack and stroke, and prevent the clogging from getting worse. Screening for PAD is not only important for the arteries of your legs but because it could reveal risks of blood flow restriction in other arteries we do not look at or screen for, such as the arteries of the heart.
Since the PAD screening is done while you are at rest, some issues may go undetected. You should always discuss your screening results with your physician or other health care practitioner and discuss not only the results but any other symptoms you are experiencing.
Diabetes or other metabolic syndromes can increase your risk of PAD. Smoking (past or present) is also a risk factor for PAD. Your physician is the best resource to discuss your results, symptoms and concerns and to determine the most appropriate follow-up plan.
Who should get screened for peripheral artery disease?
Every adult aged 50 and older should get screened for PAD annually since age is a factor in developing the disease. If you have any of the additional risk factors we mentioned, you should consider getting screened earlier.
As a reminder, any adult 40+ with a history of smoking, high cholesterol, obesity, family history of cardiovascular disease or stroke, diabetes and high blood pressure should get screened as well. The test itself only takes a few minutes and will give you vital information about your health.
If the technician determines that you are at a high risk for PAD, or believes you have developed a case, the best thing to do is to speak with a doctor as soon as possible. PAD is treatable and a physician will be able to recommend a treatment plan that can reverse the effects. Also, the longer PAD is left untreated, the more likely it is that more serious side effects will develop.
The Bottom Line
Peripheral artery disease (PAD) is when the arteries carrying blood to your legs and feet get clogged with plaque, restricting blood flow. It sometimes causes pain in your feet and legs, but if left untreated, it can cause tissue death and in extreme cases, require amputation. If you’re over the age of 50—or if you’re over 40 and have additional risk factors—you should definitely get a quick, non-invasive screening to see if you’re at risk of having PAD.
Peace of Mind with Life Line Screening
At Life Line Screening, we have years of experience helping people prevent major medical issues with vital early detection services, including PAD. In fact, screenings are our specialty. We partner with community centers to help people get quick, easy access to the screenings they want to stay on top of their health. No lengthy doctor’s visits, no complicated insurance to deal with, just convenient screenings for health-conscious people conducted by trained professionals.
Learn more or schedule a screening today at lifelinescreening.com — or give us a call at 800.718.0961. We’d love to help.
Topics:
Abdominal Aortic Aneurysm